Helping your son or daughter get through a cold can be hard enough, so making healthcare decisions for them during a crisis can seem overwhelming. Aubrey and Jason Gibson know this first-hand. Three years ago their fourth-grade daughter Aria developed abdominal pains so severe, they took her to a nearby emergency department.
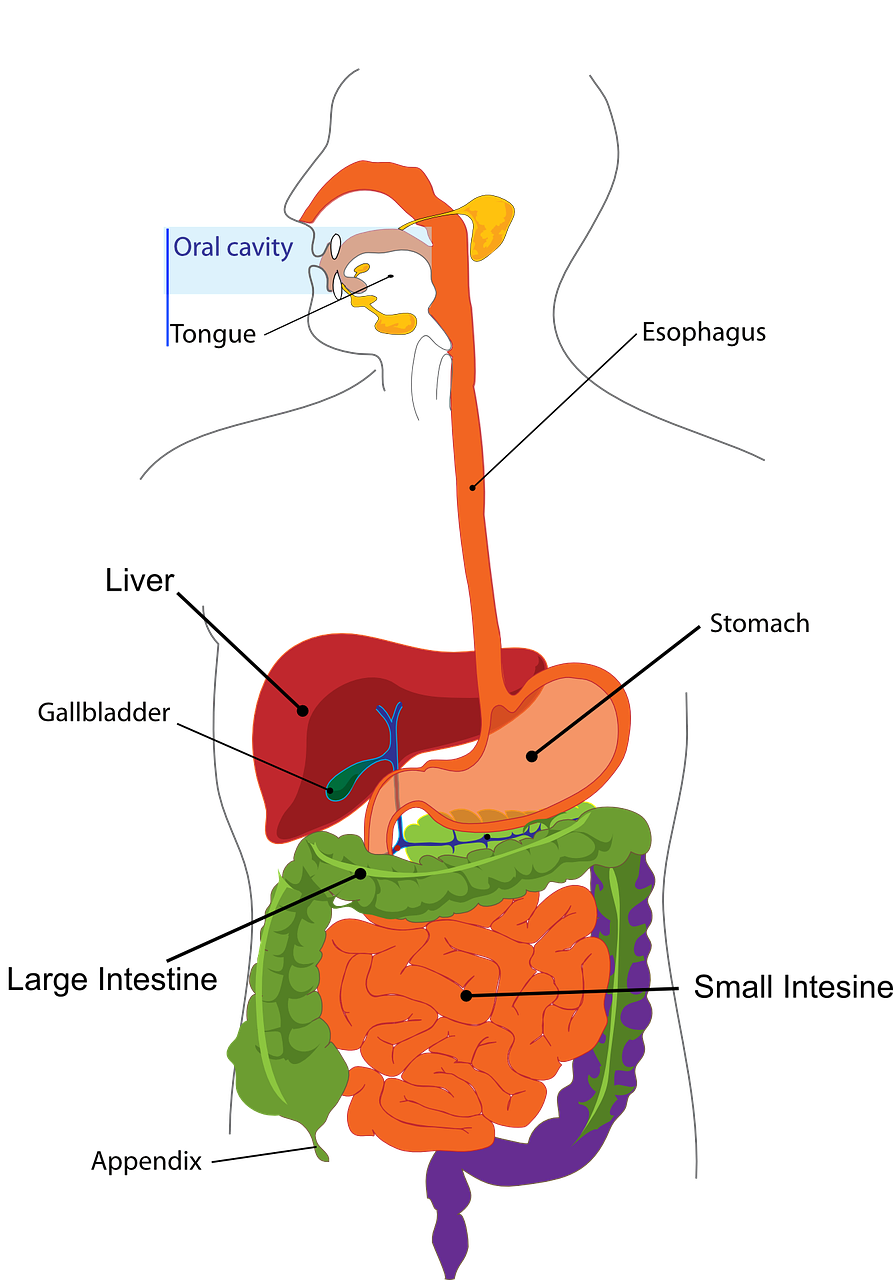
Aria had appendicitis. The doctors said the family had a choice: the standard treatment—surgery to remove the appendix—or a newer, noninvasive option, a course of antibiotics without surgery.
When a serious health crisis hits, parents naturally want to confront it with the most immediate and strongest treatment. Sometimes that’s surgery, but sometimes there are other options. With their daughter’s health at stake and the clock ticking, the Gibsons had to make a decision quickly.
After consulting with doctors, the family chose antibiotics. A factor in that decision was that the Gibsons had planned a surprise trip to Disney World in two weeks. Surgery has a one- to two-week recovery time; with antibiotics, Aria would be ready to travel in just a few days.
The family went to Disney World and experienced no problems. Aria has been healthy ever since.
Aubrey, Jason, and Aria have since worked with researchers, other families, clinicians, and insurance company representatives on a research project to develop and test a tablet-based app to help families of children with uncomplicated appendicitis quickly decide between surgery and antibiotics.
The goal of the app is to help patients and their families become more involved in their care and better prepared to make decisions. Increasingly common, such decision tools have proved effective in adult medicine, but haven’t yet been widely tested in pediatrics, emergency medicine, or surgery, notes Katherine Deans, a pediatric surgeon at Nationwide Children’s Hospital in Columbus, Ohio, and the principal investigator of the study, which is funded by the Patient-Centered Outcomes Research Institute (PCORI).
Appendicitis affects more than 70,000 U.S. children each year and is truly an emergency. Decisions about treatment must be made within hours of the first symptoms. Deans, along with her research partner and husband, pediatric surgeon Peter Minneci, hope that their testing will show that after using their app, parents will feel much more confident that they made the correct choice for their child and their family.
The researchers expect results in the summer of 2017. Minneci notes that appendicitis is a test case. If the study shows that the app is effective, they could tailor it for use in other emergency situations in pediatrics, like premature births or crises involving critically ill children in intensive care units.
You can find out more about this project and other patient-centered research funded by PCORI at www.pcori.org.